Education & Help for Loved Ones of Patients
In addition to our comprehensive, personalized treatment programs designed to restore your loved one’s physical, emotional and spiritual health, we offer therapy and various programming options to help educate, support and care for families, caregivers and friends of patients in treatment at every stage of the recovery process.


Treatment Teams
Behavioral health conditions like mood, anxiety and trauma-related disorders are complex illnesses that require a multidisciplinary treatment team with an acute knowledge of these conditions: ranging from symptoms to supportive practices. Our treatment teams consist of a psychiatrist, family therapist, nurse, case manager, alumni coordinator and other related patient support staff. A full-time internal medicine physician is also available to all our patients.
Involving Families
We know that families, friends and support people are a critical aspect of the recovery process. From family therapy and online support groups, to our Virtual Family & Friends Education Series, we offer continued opportunities for you to participate in your loved one’s recovery.
Armed with knowledge and skills, you’ll be able to serve as a resource for your loved one, and gain an understanding of their progress throughout treatment as you become an active and involved member of the process.

What to Expect
Family Involvement in Treatment
Recovering from a mood, anxiety or trauma-related disorder “takes a village.” In addition to the hard recovery work your loved one will complete with their treatment team, families are strongly encouraged to participate in the treatment process to learn about the condition and receive supportive practices and strategies. The specific goals of family involvement will depend on the pre-admission assessment process: used to develop your loved one’s individualized treatment plan.
Family Therapy
Weekly individual family therapy sessions are part of your loved one’s programming. You can expect to learn more about family therapy during admission: at that time, the treatment team will suggest times for your first family therapy session. In addition to family therapy, our Virtual Family & Friends Education Series is a weekly educational series designed for families, friends and support systems of Pathlight Mood & Anxiety Center patients.
Family involvement is particularly critical for the parents of young patients admitting into child and adolescent programs. The treatment approach for patients ages 10 through 17 is rooted in Family-Based Treatment (FBT), which empowers parents to become agents of change in the recovery of their child. Pathlight also uses Emotion-Focused Family Therapy (EFFT) for its adult patients, with core principles including emotion coaching, behavior coaching and relationship repair. We continuously work to incorporate families into care plans: delivering education regarding the challenges of mental health conditions, practice and guidance in how to encourage open and honest communication, clarity on family goals and how to create a structure to achieve them, and more.
"Coming together each week with other families, friends, and support systems who can relate and empathize with your experience helps you form a community of personal bonds and connections.”

Your First Call
When a loved one is hurting, it is often family members, caregivers, friends or other support systems who take the brave step of encouraging their loved ones to get help.
Calling the Treatment Center
If your friend or family member is struggling with a mental health condition, please call us at 877-711-1878. A member of our Clinical Assessment Team, comprised of Masters-level counselors with specialized training in mental health, will answer the call.
Getting matched with the exact support they need.
With one conversation, our mental health professionals will help your loved one better understand what they’re going through and what they need.
We will meet them where you are, listen to their story in a therapeutic setting, and match them with the level of support that meets their struggle.
How to Help Your Loved One
We know that family members and friends have questions – and lots of them. We encourage you to consider the following as you seek information about treatment:
- Do your loved one’s symptoms require intensive treatment? Be prepared to share what you know about their current and past symptoms.
- Is the illness interfering with your loved one’s daily life? Be prepared to answer questions about sleep, self-harm, eating patterns, social relationships, professional and / or academic life.
- Will a higher level of care be the best choice? A reputable treatment center will typically offer intensive supervision and support for your loved one.
- What will your level of involvement be in your loved one’s recovery? How will you receive support? A reputable treatment center provides family therapy and education throughout treatment.
If you call Pathlight Mood & Anxiety Center, our team will guide you through an assessment to help answer these questions. Your first call with a treatment center should give you sufficient information to make a sound decision regarding the care and treatment of your loved one.
If treatment seems like a viable and appropriate option, we will set up a more in-depth consultation. Our goal during these early conversations will be to create a safe space and determine the best path to recovery.
Choosing a Treatment Center
If your loved one’s illness meets criteria for our intensive levels of care, we will assess the level of support they require. ERC Pathlight provides a full continuum of care, from outpatient therapy sessions, up to and including full hospitalization. Our assessment team will review your loved one’s needs specifically and will recommend that they enter treatment at a level of care appropriate for their needs.
If your loved one is recommended for residential treatment, they will be assigned a room, most of which are shared, two-person rooms. We are proud to serve a diverse population of patients, with a foundation rooted in culturally competent programming. Adults (18 and up) are housed separately from our child and adolescent patients (ages 10 to 17), and our adult programming is separate from our child and adolescent programming.
Making the Best Decision for Your Family
At Pathlight, we work collaboratively to consider each patient’s individual needs on a regular basis, continuously assessing progress and goal setting. Our collaborative approach ensures that patients stay at each phase of treatment until they are ‘ready’ to move on to the next.
We know that change is difficult; it is normal to worry about your loved one and to have concerns about the unknown. We are here to support you, answer your questions and guide you through next steps.
While mood, anxiety and trauma-related disorders are serious conditions, we firmly believe that everyone deserves the chance to achieve a life-changing, long-lasting recovery.
Pathlight Orientation for Family & Friends
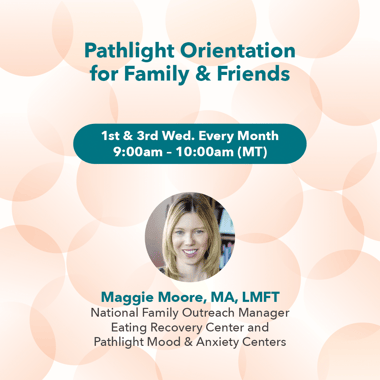
Join us virtually for the Pathlight Orientation for Family & Friends. This presentation will cover what to expect from treatment, programming basics, next steps, and Q&A.
All stages of treatment are important, but the beginning is a critical foundation to them all. The Pathlight Orientation will help establish a strong beginning, middle and end.
During the Orientation you’ll learn more about:
- What benefits each level of care offers, and how they tie together.
- Who your loved one’s treatment team is and when you’ll connect with them.
- When you can be involved, and why your involvement is important.
- How to prepare for the end of treatment, and when to start preparing.
The Pathlight Orientation is open to all Pathlight family and friends and will be hosted on Zoom.
Every 1st and 3rd Wednesday of the Month at 9:00 am MT.
Please note, you only need to attend the Pathlight Orientation one time.

Your First Day
Be proud of yourself for having the strength and courage to be here right now: supporting your loved one in treatment. You are making an enormous and critical difference by supporting your loved one on their journey to recovery.
Arriving at the Treatment Center: What to Know
When patients arrive for care at our center, our staff are trained to provide the support and care each patient needs as they enter treatment.
On the first day of treatment, your loved one will receive support to help familiarize them with the treatment center, feel safe and supported and settle in.
If you are the parent of a child or adolescent, you will be involved in the intake process and be able to meet with members of the treatment team, attend an orientation and attend groups.

Determining the Length of Treatment
You may wonder how long your loved one might be in our care. While the journey to recovery is different for each person, key markers of recovery include the following:
Mental/Emotional Stability
All distressing, harmful behaviors and any serious or acute mood disturbances will need to be understood and treated. Harmful coping mechanisms or behaviors may have included substance use, self-harm or other process addictions. Recovery involves being in a controlled, supportive environment, where patients know they are neither judged nor critiqued. In treatment, your loved one can gain space from the stresses of daily living to gain awareness, perspective and clarity. They will use this time to learn and master skills to help them regulate their mood and nervous system.
At times, insurance companies have different criteria and standards for how long your loved one can remain in treatment. While our Business Office works closely with third party payers, payers ultimately have the final say regarding the length of stay. More often than not, we are in full agreement with insurance providers regarding treatment plans and length of stay. If a situation occurs and we are not in alignment, our dedicated Business Office staff will answer your questions and help to advocate with your insurance providers.
The length of stay is very personalized and individualized. However, our median length of stay is six to eight weeks.
Where to Stay
Families choose to travel from near and far so that their loved ones can get the best care possible at our Pathlight centers.
In order to mitigate some of the stressors surrounding location and travel, we provide concierge services to assist our out-of-town patients and families. Our admissions team is available to assist you with a wide variety of needs before and during treatment.
While your loved one is in care, we often suggest that friends and family members return home to care for themselves, rest and restore. We also understand that every individual is different and personal circumstances vary. Please communicate with the treatment team if you feel that you should stay near your loved one’s treatment center. We will work with you to help make the decision that is best for you and your family.
Finding Support For Yourself
Not everyone understands what it is like to have a mental health condition, or a loved one who is sick. But by sharing your feelings and forming a community of connections with others in similar circumstances, you can feel more empowered and less alone.
It can be helpful to attend our caregiver support groups and other educational opportunities so that you can share your experience with other parents and families that understand exactly what you are going through. Our Virtual Friends & Family Education Series is a session designed specifically for families, friends and loved ones of both adult and child and adolescent patients: offering hands-on, practical information about mood and anxiety disorders, supportive practices and best methods for communication.

Tough Days in Treatment
We wish that treatment and recovery were easy. But it may be the most challenging work that your loved one – and you - have done.
We know how difficult it is when someone you love is suffering. But the only way that your loved one will be able to treat and cope with their condition — and thrive — is to do the work recommended in treatment and dedicate themselves to a full recovery.
Feeling Ambivalent About Treatment
When your loved one begins treatment, you may wonder if this is the right place for them. You may wonder if they are really "sick enough" to need help. Alternatively, you may feel a huge sense of relief.
At times, our patients and their families will ask if a higher level of care is truly necessary. We frequently hear our patients say:
- “I’m not as sick as the other patients are.”
- “I have no friends here.”
- I feel worse since coming here.”
- "They don’t know how to treat my condition(s).”
- “I’m not on the right meds.”
These statements are normal and to be expected; typically, these types of feelings will pass within a few days.
If you or your loved one feel ambivalent or unsure about the course of treatment, know that you have a choice. You can choose to work towards a long-lasting recovery, or you can choose life with a mental health condition and everything that comes with it. If you choose the path to recovery, know that full recovery will not be possible without hard work.
Resisting Treatment
Often, when it comes to young people in treatment, we encounter the following scenario: parents drop their child off at the treatment center and feel an acute sense of relief. Yet the child is suddenly left without their coping behaviors, immediately feeling overwhelmed, and frequently lacking insight into how and why they feel a certain way.
Negative experiences are normal and to be expected at some point in recovery. Tears, anxiety and anger are part of the process. But if you find that your loved one is actively resisting care, consider the following:
- Validate them. Tell them you understand how hard this is.
- Support them. Tell them that this is the right place to be.
- Encourage them. If your child continues to resist treatment, ask your child to share these thoughts and feelings with their therapist — and make sure you talk to the treatment team directly.
The Toughest Days of Treatment
In treatment, your loved one will likely experience physical sensations and emotions that they have not felt for some time. This can be overwhelming and unpleasant. We remind our patients that this discomfort is temporary, and that “it’s okay to have a bad day.” In time, the pain and discomfort will lessen and become manageable.
The first few days and weeks of treatment are inevitably challenging. In these difficult moments, remind yourself of the why: why your loved one considered treatment in the first place. It’s likely they began treatment because they were facing a severe, and possibly life-threatening, health crisis.
Please know that your loved one is safe with us. Our care facilities are designed to keep our patients physically and emotionally safe, with an environment rooted in mindfulness, awareness and connection. Their well-being will always be our top priority.
Making Progress in Recovery
Recovery does not always occur in a straight line; in fact, it is rarely linear. There are often setbacks, in addition to celebrated successes, on the path to recovery. Your love and support will be crucial to help your loved one navigate the rough patches.
If you are the parent of a child who is ill, you may want to do what you can to “fix” your child’s problem — and you may want to fix things quickly. Yet the truth is: you cannot fix it for them. Instead, you can support, validate and encourage them to do the hard work of treatment. Their job is to focus on getting better and your job is to support them.
Supporting Your Loved One in Care
Treatment is often overwhelming and emotional for everyone involved. It takes time and a lot of work to process these hard changes. One of the best pieces of advice we can offer is that you talk openly with the treatment team and trust the clinical guidance. Moreover, our family programming will give you the skills to support your loved one not only during the treatment process, but also when they return home to life outside treatment.

Life After Treatment
Continuing in Recovery
When a patient discharges from treatment, it is normal for both patient and caregiver to worry or feel overwhelmed. As a friend or family member, you play an important role in the recovery support process after your loved one returns home from Pathlight.
When people transition back to life outside of treatment, they realize how much of a cocoon the treatment setting was. In the treatment center, your loved one has been surrounded by experienced clinicians and professionals that specialize in treating people with mental health conditions. Patients can talk openly about feelings and behaviors with people who understand — including people who are going through many of the same things.
Keeping in Touch
A strong support system will be critical for your loved one after treatment ends. Our clinician-led Alumni and Family Liaison Team is here to help you and your loved one create and maintain a support system.
Our Alumni and Family Liaisons follow up with patients after treatment ends or follow up with parents of patients under the age of 18. Email check-ins will occur at different time periods: at seven days, thirty days, three months, six months and one year after discharge. Our goal during these check-ins will be to see how you are doing, help you find resources and answer any questions you might have.
One of the maximum benefits you can offer your loved one is continued learning about the unique challenges they will face at home in recovery. We offer many avenues of support to help you do this:
- Online webinars provide education and support in the comfort of your own home.
- A list of resources and online support groups helps you connect with others.
- Our blog offers continued support and education, inclusive of lived experience stories from others who have combatted mental health conditions.
- Invitations to continue attending the Virtual Family & Friends Education Series.
- Participation in Recovery Day, a day to celebrate all the hard work you and your loved one have done in seeking better mental health.
You are always welcome to reach out to us via phone call or email. For us, support does not end at the time of discharge from treatment.
Transitioning Home
Your loved one has made a difficult and brave decision to do the hard work required in treatment. We ask you to support them as they continue this challenging work at home.
We encourage your involvement in the transition home, which will be progressive and in phases. Your loved one will first come home at night and on weekends before they permanently return home.
Once they are fully discharged, we will recommend ongoing outpatient care.
Transitioning to Outpatient Care
Your loved one has made a difficult and brave decision to do the hard work required in treatment. We ask you to support them as they continue this challenging work at home.
We encourage your involvement in the transition home, which will be progressive and in phases. Your loved one will first come home at night and on weekends before they permanently return home.
Once they are fully discharged, we will recommend ongoing outpatient care.
Dealing with Relapse
Should your loved one experience a relapse or need help at any time after discharge, please contact us:
- Call our Clinical Assessment Team at 877-711-1878 or via email at [email protected].
- Email the Alumni Team at [email protected].
Starting treatment and achieving full recovery is not a straight line. Your loved one may be in treatment more than once. Recovery may even take many years.
Maintaining Hope
The road to recovery can be a long and arduous journey. We are with you for the long term. At any point after discharge, if you need assistance or resources, please contact us. We will be here for you and do our best to help you get the assistance that you need.

Stay Connected with Your Recovery Community
Are you or a loved one on the path to recovery? Our new opt-in form enables you to stay connected with our team and continue to receive support after discharge and throughout your or a loved one's recovery journey. By signing up, you'll receive the latest free resources, including access to support groups, upcoming events, educational materials, and more.
Support for Children and Adolescents After Treatment
Your child will gradually spend less time in the treatment program and more time with you in “real-life” situations before they return home. Family meals, outings and passes will become available as your child progresses throughout the phases of treatment.
We will ask you to help create your child’s “aftercare plan” for the return home. If your child is in residential care and you have resources in your home area to support ongoing care, we will work with you to evaluate all available treatment options.
We will explain how to monitor and support your child as they begin to navigate life outside of treatment. Please contact us if your child is engaging in any harmful behaviors or maladaptive coping mechanisms.

Supporting Family Members and Loved Ones in Treatment
How do you know if your loved one is making progress in treatment?
If your loved one is in our child and adolescent programming for patients under the age of 18, you will be involved in weekly family sessions. We will regularly review both their progress and challenges. If your loved one is an adult, we will also keep you updated on their progress — as long as they have chosen to have you involved in the process.
Family Therapy
Our family therapy program is an essential part of treatment. In family therapy, we address family dynamics, communication patterns, stressors within the family and other experiences that affect you, your loved one or other family members.
Family therapy helps caregivers who will support the patient after discharge. Goals include delivering education, learning new skills and teaching families how to best support recovery.
For children, family therapy will include custodial parents or guardians and other adults they may identify. Family therapy is scheduled at least once weekly for children in our care and their parent(s).
Adults and their families can also have a weekly family session; this may include a life partner, spouse, friend, adult children and the person or people who will support their care post-discharge.
Your loved one’s primary therapist will run family therapy sessions. This person is the liaison between the family support members and your loved one’s treatment team. The primary therapist will provide you with updates on progress and challenges and can help arrange times to talk to other team members, if needed.
Mental health conditions often stem from issues within the family and can have effects that impact other family members. For this reason, among others, our family programming is a crucial aspect of treatment.
Family Support and Education
We provide ongoing support and education to families, caregivers, support people and friends. If your loved one is in residential or PHP level of care, there will be family support programming scheduled. Intensive outpatient levels of care may have family education offered. Our Virtual Family & Friends Education Series is open and available to all family members, friends, caregivers and support systems of Pathlight patients: whether you have a loved one in treatment or are simply seeking more information. Family members, caregivers, and support people are also welcome to join the Mood & Anxiety Family and Caregiver Support Group at any stage of their loved one’s treatment.
Multi Family Groups
These support and educational groups are designed to provide you with the information needed to be an effective recovery support for your loved one. Multi family groups are facilitated by our highly trained staff, offering you the chance to gain understanding, support and validation from other family members who are working to understand and support their loved one’s recovery. While some groups may include your loved one, most frequently, we seek to set up a safe, supportive space for you to share and discuss concerns.

Virtual Family & Friends Education Series
We know that when someone you love is in treatment, you may feel lost, alone or powerless. At Pathlight, we offer you the necessary tools to be a strong support for your loved one in recovery. We have developed a suite of hand-picked resources, recorded presentations and events that can help you learn more about your loved one’s condition, and how to be an effective part of their recovery.
Our Virtual Family & Friends Education Series is hosted by our clinical leaders from across the country, delivering practical, hands-on knowledge of what you can do during and after treatment to support your loved one. These sessions include signs, symptoms and supportive practices related to mental health conditions, in addition to communication strategies to engage with your loved one.
Working Together to Achieve Recovery
Mood, anxiety and trauma-related disorders don’t just affect patients — they also impact family members and friends. This means that you play a very important role in your loved one’s treatment: you are an integral part of their recovery.
As you support your loved one — validating, listening to and emphasizing with them — we will validate, listen to and empathize with you, too. Let us know if you have any questions or needs while your loved one is in treatment.
A Special Note for Parents
We sometimes recommend that parents take a break from visiting as your child embarks on their recovery journey. These breaks can help foster independence and allow you to focus on yourself by practicing self-care, and focusing on other family members. If you have questions about visits, please consult with your treatment team.
